Consultations in the prenatal period
At Around 7 weeks you have your first echo at Focus. Call us so we can make that appointment for you as soon as you are pregnant.
Your first visit at our practice will be when you are around 8 weeks pregnant. It takes about 45 minutes. At this appointment we will get to know you better and will ask you questions about the health of you and your family. At www.pns.nl you can find the list of questions. Is it not your first pregnancy, then we want to hear more about that pregnancy, birth and postnatal period of your ither children. We will give you information about what to eat (check the Zwangerhap app.) We will give you all the information about the NIPT and de 13 and 20 week echo. At our Breda location we will also make an echo. When you are 10 weeks you will have the next echo/ultrasound. It’s is called a “ termijn echo” and will determine the due date. Please call us the next morning after the echo and let us know this due date so we can order the 13 week echo.

At 12 week you come to the praxis again for check-up. We then give you the lab form for the NIPT if you want to do this test.
Prenatal consultations are in week 8-12-16-19 (echo)- 23-27-30-33-36-38-39-40-41.
Every consultation we check your blood pressure and weight. We check if the baby is growing well and we listen to the heartbeat of the baby. At our Breda location we check it with our new echo machine.
Questionnaire on your health and that of your family:
Do you consider yourself healthy or do you ever visit a GP or specialist?
If so what diseases do you have or what have you had surgery on?
Do you have any congenital defects yourself?
Have you ever suffered from thrombosis, bladder infections, fungal infections, anaemia, blood transfusion or chicken pox?
Have you ever had a negative sexual experience or experienced domestic or physical violence?
Have you ever been treated for an STD?
What medications are you taking?
What allergies do you have?
Do you smoke and/or use alcohol or drugs?
Have you ever seen a psychologist or a psychiatrist?
Is your partner healthy?
Does your partner smoke or have allergies?
Does he/she have birth defects?
The health of both families
Does either of your families have a congenital or hereditary condition? For example, syndromes or intellectual disabilities, spina bifida or skull, disorders of brain, nervous system or muscles, lip and/or palate cleft, heart defects, sickle cell disease, thalassemia or haemophilia (blood diseases) etc?
Do any of your parents or brother/sister have diabetes or high blood pressure?
To do list
Before 16 weeks:
- Subscribe for Kraamzorg/postnatal care. This is care by a specialized nurse. She helps during labor and takes care of you and your baby the first week after birth. She checks mother and baby and helps with bathing and breastfeeding. Call them around 12 weeks.
- Blood test should be done between 7 to 10 weeks. Preferably in the hospital Amphia. At your first visit we will give you a lab form.
- Contact “mothers for mothers”. You can help other women by collecting your urine.
Before 24 weeks:
- Subscribe for a pregnancy course. This course will help you when giving birth.
- Erkenning/recognition . If you are not married or you don’t have registered partnership, you have to go to the City hall to let them know officially who are the mother and father of the baby and how it will be named.
- You have to tell your employee at least 3 months before the due date that you are pregnant. Maternity leave starts max. 6 and minimal 4 weeks before de due date. You can have 16 weeks maternity leave. If delivery takes place early, you still have 16 weeks leave.
Before 30 weeks:
- Kraampakket or maternity package. Inform your health insurance that you are pregnant. They will send you the box with items for delivery and maternity period.
- Het kraamzorg bureau will plan a home visit for intake.
Before 37 weeks:
- Bed raised with bed-blocks (bed around 75cm or higher, also when you want to give birth in the hospital) in the home care shop.
- Small suitcase with your clothes and a set for the baby. Diapers and sanitary towel is available in the hospital.
Prenatal screening
We have 3 tests, the NIPT and 13( ETSEO) and 20 (TTSEO) week echo. When you visit us for the first time we will explain what these tests mean. Please visit www.pns.nl and read more about these texts in your own language.
NIPT
This is a blood test. It costs around €175. You have to pay this before you go to the hospital to do the test. The test can be done after 11 weeks pregnancy. In your blood they can find chromosomes from the placenta. They look a lot like the chromosomes of the baby. If they find a defect in one of the chromosomes, it is possible that your baby is not okay. We will arrange a consultation with a specialized doctor for extra tests.
If you want to do the NIPT we will give you the lab form when you visit us in your 12th week. It will take 14 days to get the results.
The NIPT costs 175 euro. Sometimes insurance will pay these costs. Check with your insurance company. Starting from April 2023 it will be free.
ETSEO or 13 week echo
This echo needs to be done between 12+4 weeks and 14+4 weeks. So call us in the morning when you know your due date, then we can order the ETSEO. The baby is then only 5 cm small they cannot detect as much as with the SEO, but it is possible to detect some malformities. Because this echo is still a scientific study there will be no costs. They do not look at the gender of the baby. If the position of the baby is not good to view everything the echoscopiste might want to do a vaginal echo.
TTSEO or 20 week echo
With this echo we check if your baby is healthy and if there are no malformations. We will measure the baby to see if it grows well and if you have enough amniotic fluid. If the ultrasound technician finds something unusual, she will contact us and then we will call you. Most of the time we will arrange a consultation with a doctor to see what steps are necessary.
If the TTSEO is good it does not automatically mean your baby is healthy , because with ultrasound we cannot look into the cells, we can only check the surface of cells.
Check www.pns.nl for more information.
Life tide advice in pregnancy
Nutrition and pregnancy
It is very important to eat healthy food when you are pregnant. You don’t need to eat for 2. At the site of the “nutrition center” you can read what is good and not good to eat. Install the app “Zwangerhap”, it gives information about all kind of nutrition.
It is good to take extra vitamins like Foliumzuur ( Folic acid) or vitamin B11. Start 4 weeks before or if you didn’t know in the beginning of pregnancy. It will help the neurological development and gives the baby a smaller chance of getting an open spine or back. Continue to take the tablets till week 10 to12.
Take 10mgr vit D. It will help the absorption of calcium. This is needed for good bones of the baby. Vit D is also made by the sun on your skin and it is in fatty fish and butter products. You can also start this before pregnancy.
Your blood volume increases when you are pregnant. Iron helps increase the blood. Its in green vegetables, red meat, whole wheat bread Vit C will help the absorption of Iron. Milk on the contrary is not good for the absorption.
We will check the Iron level in the beginning and around 30 weeks.
Your weight
What is a healthy to gain in pregnancy? At your first visit we will determine your BMI ( weight compared to height)
| BMI < 18,5 | 12,5 to 18 kg |
| BMI between 18,5 and 24,9 | 11,5 to 16 kg |
| BMI between 25 and 29,9 | 7 to 11,5 kg |
| BMI > 30 kg | 5 to 9 kg |
If you grow more than you should, look at your eating habits. If you gain a lot of weight the risk of getting, diabetes, high blood pressure or more problems during labor will increase.
Medication & pregnancy
Ask your doctor which medication you can safely continue to take in pregnancy. You can also ask the pharmacist or midwife for advice.
Alcohol & pregnancy
Do not drink alcohol when you are pregnant. Even a small bit can hurt your baby. If you drink regularely your baby can get ‘foetal alcohol syndrome’. The baby then will get physical fysiek en mental retardation. Ask for help if you don’t know how to stop. There are courses that can help you.
Smoking & pregnancy
Do not smoke when you are pregnant. Even when it is too difficult to stop smoking, you will help your baby by smoking less. When you smoke your baby gets less oxygen and more carbondioxide. This will also give stress to the baby. Smoking will make your baby smaller and you might get in labor too early.
Look at www.stivorno.nl for aid.
Drugs & pregnancy
Do not use drugs. Soft-and hard drugs can give severe problems for your baby.
Hazardous substances & pregnancy
If you want to paint the room of your baby use water based paint and make sure the room is well ventilated. No problem if you want to color your hair. If you work with radiation or rontgen or ither hazardous substances , talk to your employer to change work.
Sport & pregnancy
It is good to sport when you are pregnant. Your health will be better. Your muscles will stay strong. Giving birth will be easier and recovery after birth will be quicker.
With contact sports you can get kicked in the belly, so try to minimize that risk. When you exercise you belly muscles don’t strain the straight muscles too much.
It is fun and healthy to join a course with ‘ Zwanger and fit ’ or ‘ Mominbalance ‘.
Toxoplasmose & pregnancy
This is a parasite that can be found in the feces of cats and in meat that is not well cooked.
Contamination can cause a miscarriage or malformation. So avoid direct contact with cat litter, wash fruits and vegetables and cook meat thoroughly. Put on gloves when you work in your garden.
Travel & pregnancy
We can give you a ‘Fit to fly’ declaration the week before you fly. Inform at your airline how late in your pregnancy you are allowed to fly.
Work and pregnancy
Some work can be a hazard for your pregnancy. For example when you work with chemical substances, radiation or physical hard work. Talk to your employer and ask if you can change work or have more breaks. If necessary we can help you.
Overdue
Five options
Every person is unique and so is every birth. Some babies come very early in pregnancy, others stay for a long time. Some come quickly and some take their time. As healthcare providers, we work with you to find what is needed to make the process as safe as possible for you and your baby. Many babies are born between 41 and 42 weeks. So it is a normal gestational age. Sometimes babies stay in longer than is good for them and we would like to help these babies come earlier. The complicated part is that we don’t know which babies these are.
All the information we receive comes through the mother: how she is doing, how healthy she is, how she feels, the contact there is with the baby, the baby’s growth and the baby’s movements. Every woman experiences this in her own way and this is not always easy to measure. That is why we also use figures from studies done on other pregnant women. It is important that you make a choice that is right for you. This information leaflet shows you the options we offer.
First read the consultation card you received from your healthcare provider. It lists the main pros and cons of the choices you can make.
In this folder you can read about the possibilities in your region with figures that can help you make a choice.
There are four options
- Waiting for labour to start on its own.
- Membrane sweep / ‘strippen’ (a number of times).
- Having your waters broken in hospital.
- Foley bulb induction
Wait
Waiting for labour to start on its own is a safe choice. However, it is important that your pregnancy has gone without complications, your baby has grown well and you feel your baby moving well every day. You can have extra check-ups if you like. If you have not gone into labour at 41 weeks, the chances of labour starting on its own before 42 weeks are about 64 in 100 (see diagram opposite). You are less likely to have interventions during labour and be handed over to medical providers in the hospital. You can also choose where you want to give birth. Besides, every week in the womb contributes to better brain development of the baby.
Membrane sweep (strippen)

The chances of giving birth are increased if the midwife releases a small piece of membrane from the uterine wall during a vaginal examination. This is called ‘strippen’. There must already be some dilation to reach the membranes. As the membranes detach a little bit, hormones are released. These hormones can be the last step to start labour. If ‘strippen’ works, you will have contractions within 20 hours. Strippen can be repeated after a few days.
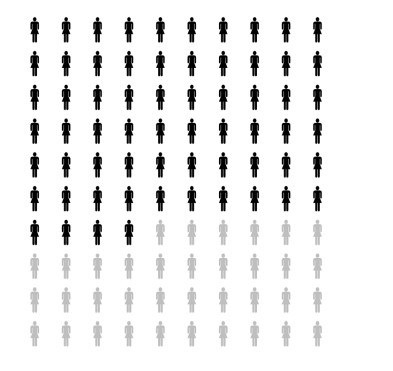
Labour is more likely to start on its own before 42 weeks in pregnant women who get a membrane sweep: 68 out of 100. Pregnant women who do not get a membrane sweep are 54 out of 100. An introduction is therefore needed less often if you get a membrane sweep. These figures come from a study where a membrane sweep was done every day or every other day from 41 weeks.
Labor induction in hospital
If labour does not start and you have it induced with medication in hospital, it is called an introduction. You can read more about this in the consultation card you received. In the information below, you can also read and see what the figures were in the Netherlands for pregnant women who were initiated at 41 or 42 weeks.
break the membranes
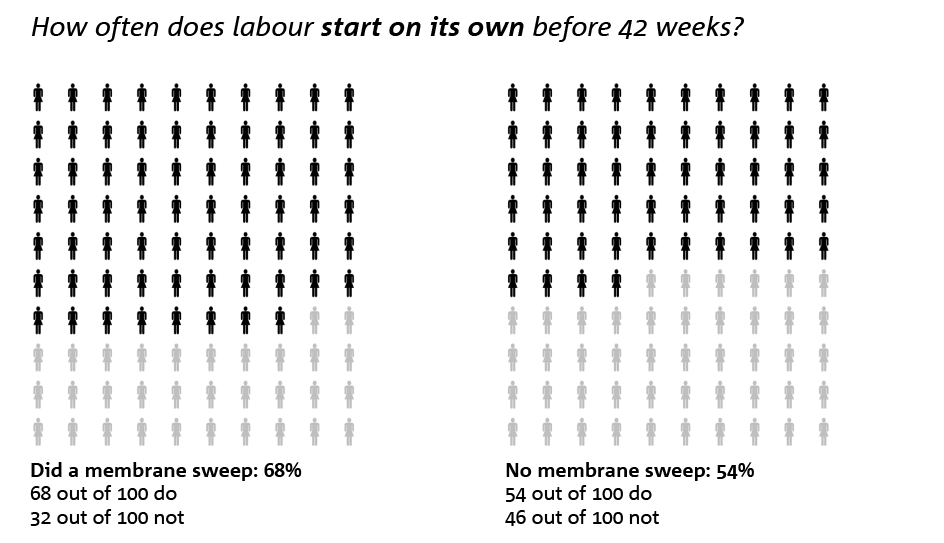
If your pregnancy keeps getting longer, there may come a time when you want to have your labour induced. The hospital midwife may try to break the membranes. The waters can only be broken if you already have some dilation. In 85 out of 100 pregnancies, labour then starts on its own (see diagram opposite).
In addition, medical interventions such as tranquillisers or painkillers are less often needed and you are more likely to be able to give birth at your preferred location.
If the waters are broken and it turns out that the baby has defecated in the amniotic fluid (meconium-containing amniotic fluid), the baby’s heart tones are additionally monitored with a cardiac video.
Foley bulb induction (balloon catheter)
If it is not yet possible to break the membranes and you want to be induced, the cervix will have to be prepared first. This is done by inserting a thin catheter into the cervix and then injecting fluid into the catheter, creating a balloon catheter that will stretch the cervix. After one or more days, the balloon catheter will fall out of the cervix and the hospital midwife can break your waters. Placing a balloon catheter is very safe. Little research has been done on the likelihood of contractions starting on their own. In a small group of pregnancies where this was already used once in the Netherlands, 87 out of 100 pregnancies went into labour by themselves after the waters broke. Among the pregnant women who went into labour for the first time, 23 out of 100 gave birth after balloon induction without the need for inducing contractions. Among the pregnant women who had given birth before, 48 out of 100 gave birth. Further research is yet to clarify exactly how much chance you have of giving birth without intervention after balloon catheter insertion.
Dutch situation
The numbers you see below are from the INDEX study. This was a study conducted in the Netherlands. In this study, half of the pregnant women were assigned by chance to a group in which an introduction was planned at 41 weeks. The other half were assigned to a group in which an introduction was scheduled at 42 weeks. The choice you get to make is at what point you want to be initiated from 41 weeks.
This could be at 41 weeks, somewhere between 41 and 42 weeks, at 42 weeks, or after that. The choice is yours and in consultation with your healthcare provider and may also depend on the amount of space in the hospitals.
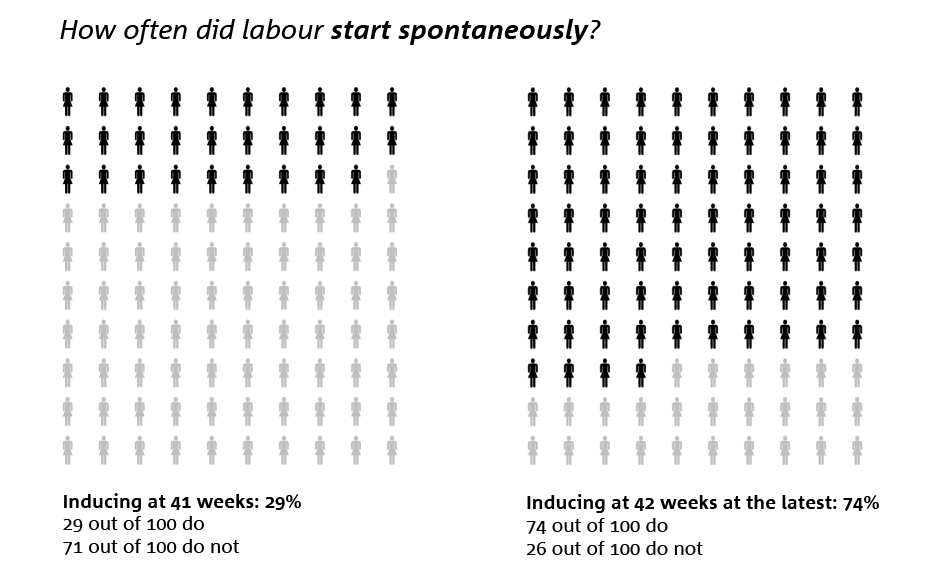
Of the pregnant women who were assigned to be initiated at 41 weeks, in 29 out of 100, labour started on its own. Among pregnant women who waited until 42 weeks, 74 out of 100 went into labour on their own.
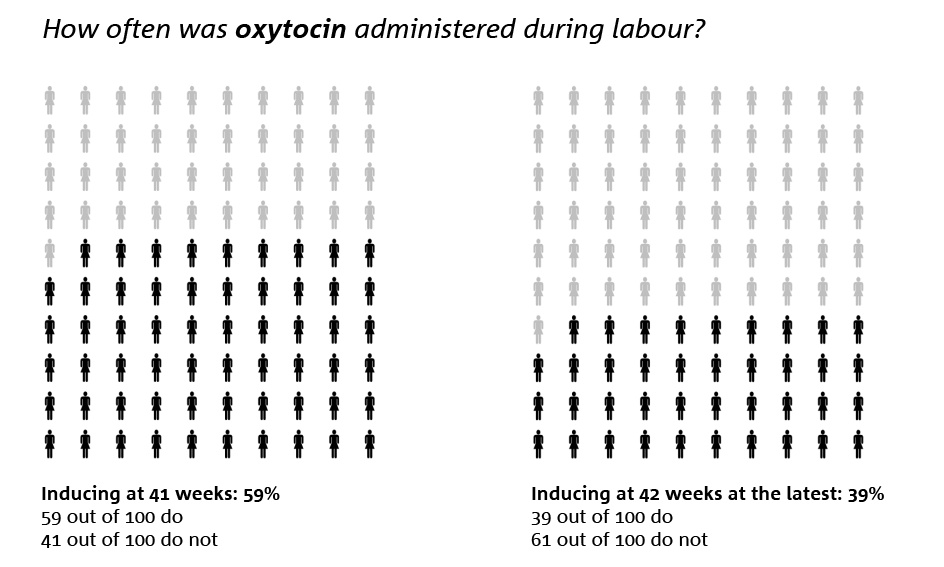
Oxytocin is a drug that induces or makes contractions stronger, and like any drug, it also has drawbacks. Oxytocin was more often given to pregnant women who were due to be initiated at 41 weeks, 59 out of 100. This was the case for 39 out of 100 pregnant women who were due to be initiated at 42 weeks.
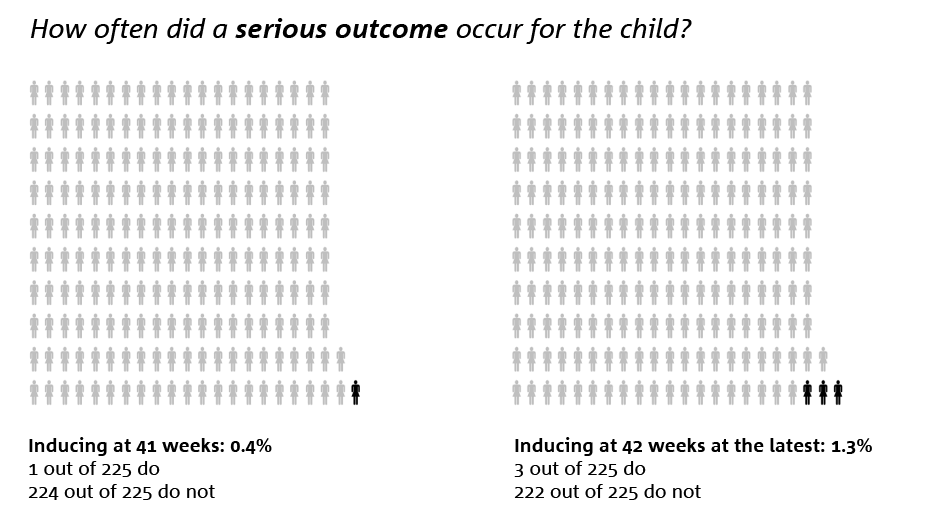
Among pregnant women who were to be initiated at 41 weeks, serious outcomes for the child were slightly less frequent, at 1 out of 225. Among pregnant women who waited until 42 weeks, it was 3 out of 225. This difference could be due to chance, as it involved few children. A serious outcome for the child could include a poor start, death, damage to the baby or admission to intensive care.
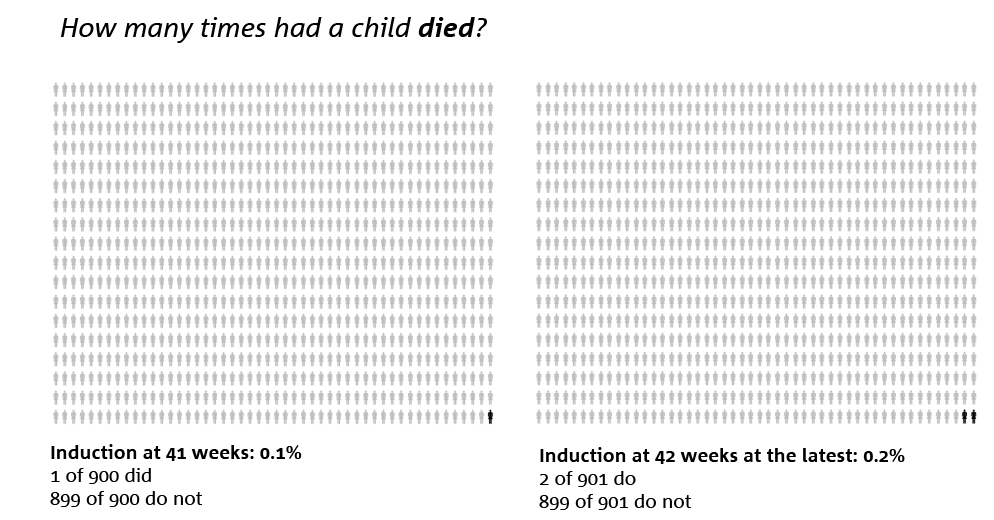
Of the 900 pregnant women who were due to be initiated at 41 weeks, 1 baby died. Of the 901 pregnant women who waited until 42 weeks, 2 infants died. This difference was probably due to coincidence. In fact, the number of children dying was very low in both groups.
If you have any questions, feel free to discuss them with your obstetric care provider. There is no right or wrong decision about whether to initiate or wait. Trust your own wishes and preferences.
Useful websites to visit are:
Annature.nl
Deverloskundige.nl